For International Overdose Awareness Day, Natalie Davies examines the role of ‘street’ and prescribed benzodiazepines in drug-related deaths in Scotland, which last year reached the highest number since records began.
On 30 July 2021, the National Records of Scotland published figures on drug-related deaths in 2020. Of the 1,339 reported in Scotland that year, 93% involved more than one drug, 89% involved opioids, 73% benzodiazepines, 37% gabapentin or pregabalin, and 34% cocaine.
Opioids have consistently been the main drug implicated in drug-related deaths in Scotland, averaging 88% between 2008 and 2020, and reaching highs of 91% in 2009 and 2010.
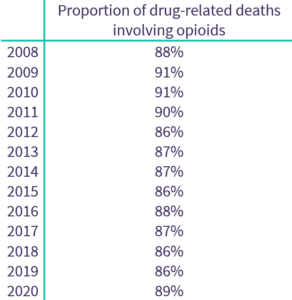
Source: National Records of Scotland (2021)
Benzodiazepines, a group of drugs originally designed for use in the medical treatment of anxiety and insomnia, have not always been such a strong feature of Scotland’s drug death stats. Between 2008 and 2015, the number of benzodiazepine-implicated deaths sat below 200 per year (averaging 27% of total deaths), but increased dramatically thereafter with 426 in 2016 (49%), 552 in 2017 (59%), 792 in 2018 (67%), 902 in 2019 (70%), and 974 in 2020 (73%).
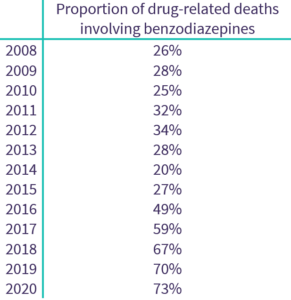
Source: National Records of Scotland (2021)
Most of this rise seems to be due to ‘street’ benzodiazepines: “illicit, unregulated copies with terrifying variances in potency”. In “Tackling benzodiazepines and their role in Scotland’s drug deaths”, the Drug Deaths Taskforce explained why these non-prescribed or non-prescribable drugs pose additional risks:
“These new drugs can be many times more concentrated and potent than those before – in some recorded cases 50x stronger – and with misleading or non-existent labelling and packaging. Many overdose incidents will be the result of an effect far beyond intended use. Equally, the times some take to have an effect – the half life of the drug – will also vary, some taking longer and opening up the further risk of double-dosing through insomnia or impatience.”
The use of ‘street’ benzodiazepines was recorded in 303 drug-related deaths in 2016, 423 in 2017, 675 in 2018, 823 in 2019 and 879 in 2020. As a proportion of total benzodiazepine-implicated deaths, ‘street’ benzodiazepines were recorded in 90% in 2020, compared with 30% five years earlier, and 0% five years before that.
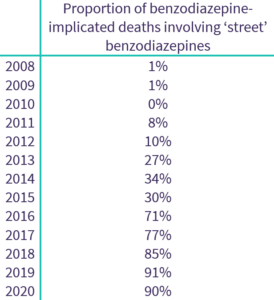
Source: National Records of Scotland (2021)
What makes benzodiazepines and opioids such a deadly combination?
When someone has an opioid overdose, they experience difficulty breathing (known as ‘respiratory depression’), which can prove fatal without urgent intervention, including rescue breathing, cardiopulmonary resuscitation, and administration of naloxone. The use of benzodiazepines, which have a muscle-relaxing effect, in combination with opioids, can increase the likelihood of a fatal overdose by further supressing breathing.
In contrast, when someone overdoses on a stimulant drug (e.g. speed, cocaine or ecstasy), they experience an increase in their heart rate, blood pressure, body temperature and breathing, which can lead to a seizure, stroke, heart attack or death. However, as the Drug Deaths Taskforce warns: “Some people might think this will help to counteract the effects of opiates and sedative drugs – it doesn’t. Instead, it puts additional stress on the circulation and can cause cardiac arrest.”
Scotland’s drug-related death rate stands at over 3.5 times that for the UK as a whole (figures available for Northern Ireland, England and Wales), and is higher than that of any European country (see European Drug Report). Addressing the role of benzodiazepines includes curbing the availability of the drugs – both those that are prescribed and make their way onto the illicit market, and those that are manufactured illegally to replicate the effects of prescribed drugs. It also includes supporting harm reduction initiatives.
The video below (click here to watch on YouTube) was produced by the Scottish Drug Deaths Taskforce, and explains why ‘poly-drug use’, and in particular the combined use of benzodiazepines and opioids, increases the risk of overdose, and how harm can be reduced, for example through services using non-fatal overdoses as an opportunity to engage with people who use drugs, trying to resolve underlying vulnerabilities such as trauma and anxiety, and testing drugs to see what is in circulation:
More information about the work of the Drug Deaths Taskforce can be found on their website.
This article was published to mark International Overdose Awareness Day – an annual reminder of the public health crisis of drug overdose deaths, and an opportunity to promote evidence-based responses.
The opinions expressed in this post reflect the views of the author(s) and do not necessarily represent the opinions or official positions of the SSA.
The SSA does not endorse or guarantee the accuracy of the information in external sources or links and accepts no responsibility or liability for any consequences arising from the use of such information.

